ARRS Case of the Week
BREAST IMAGING
Case Author: Beatriz Adrada, MD, The University of Texas M.D. Anderson Cancer Center
History
34-year-old woman with strong family history of breast cancer undergoing MRI.
Findings
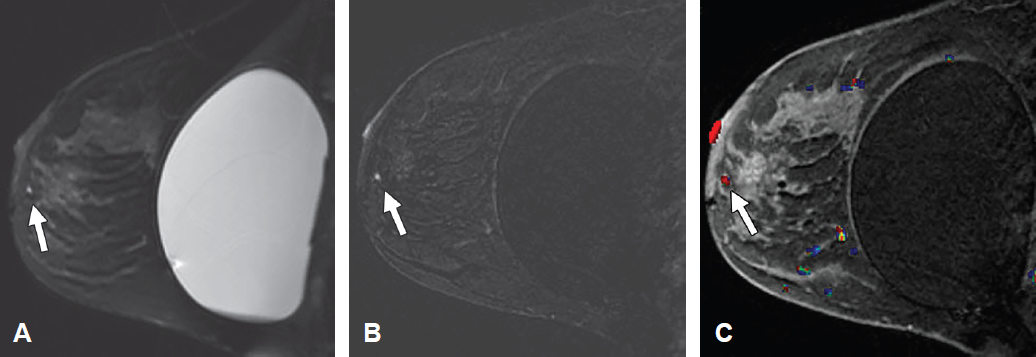
Sagittal T2-weighted fat-suppressed MR image (A) and contrast-enhanced T1-weighted images without (B) and with (C) color overlay show an enhancing focus with high T2 signal intensity and washout kinetics (arrow).
Differential Diagnosis
- Fibrocystic changes
- Invasive ductal carcinoma
- Papilloma
- Lymph node
Correct Diagnosis: Papilloma
Kinetic assessment is the description of enhancement characteristics during injection of contrast medium. The shape of the time–signal intensity curve is important in characterizing enhancing lesions. There are two phases. The initial phase depends on the slope of the line from time zero, and it can be slow, medium, or fast (“rapid” in the 4th edition of BI-RADS). The second or delayed phase displays the second part of the curve, and it can be persistent, plateau, or washout.
The kinetic predictors most associated with malignancy are rapid early enhancement followed by a washout curve in the delayed phase. Kuhl et al. reported finding cancer in 87% of lesions with any washout. Heterogeneity of kinetics is common. The more suspicious result should be used.
Patients at high risk of breast cancer are those with a lifetime risk greater than 20% according to risk assessment tools. They have a known BRCA1 or BRCA2 gene mutation, a first-degree relative who is a BRCA1 or BRCA2 carrier, and a history of radiation therapy to the chest between the ages of 10 and 30 years, Li-Fraumeni syndrome, Cowden disease, or Bannayan-Riley-Ruvalcaba syndrome. Patients at high risk should undergo MRI and mammography every year.
Although lesions with washout kinetics are suspicious for malignancy, as many as 6% of benign lesions can also have washout kinetics. Among the benign lesions with washout kinetics are normal lymph nodes, papillomas, fibrocystic changes, and fibroadenomas.
Suggested Readings
Kuhl CK, Mielcareck P, Klaschik S, et al. Dynamic breast MR imaging: are signal intensity time course data useful for differential diagnosis of enhancing lesions? Radiology 1999; 211:101–110
Saslow D, Boetes C, Burke W, et al. American Cancer Society guidelines for breast screening with MRI as an adjunct to mammography. CA Cancer J Clin 2007; 57:75–89