The Time Has Come: Interactive Multimedia Radiology Reporting

|
Cree Gaskin
Professor and Chief, Musculoskeletal Imaging and Intervention; Vice Chair, Clinical Operations and Informatics; Associate Chief Medical Information Officer University of Virginia Health System |
Read anything on the internet today and you can expect to find enriched content typical of digital communication—pictures that help tell the story, text formatting that calls attention to key information, and hyperlinks that connect us to additional content with just a click. Such features improve the experience of the reader, resulting in faster and clearer communication.
How about your radiology report? Does it do that? Probably not. Even though it’s digital, it’s likely a static plain-text-only document, just like an old newspaper. It’s surprising really, especially when you consider all the existing digital advancements within our field and the importance of the report itself to our specialty. The report is the primary means by which we, the diagnostic radiologists, deliver clinical care. And yet the formatting of our reports remains archaic.
Fortunately, times are changing. Collaborations between vendors and radiologists have led to recent advancements in technology that support interactive multimedia reporting, or the ability to create imaging reports with enriched content and better connections to the images.
The idea of a multimedia report is not new. Authors in the mid-1990's described preliminary systems for multimedia radiological communications, but over time neither proved practical or impactful enough for widespread adoption. In recent years, several independent groups of authors reported that adding images to reports would add value, following the old adage that “a picture is worth a thousand words."
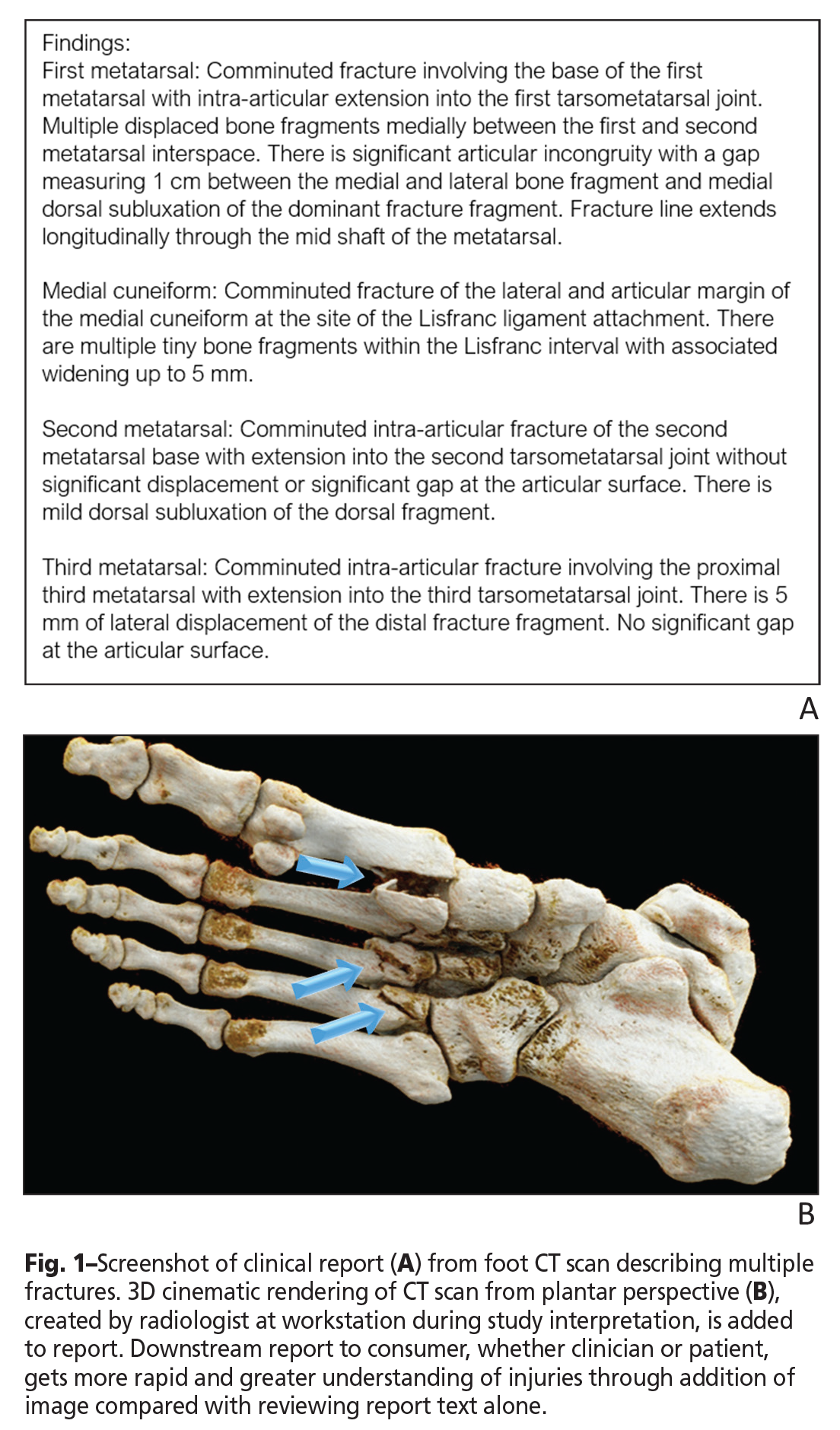
It is easy to see how adding key images to the report can help us communicate better, especially when summarizing a complex study such as a CT scan (Fig. 1). But there are practical challenges, both technical and cultural, to implementing this simple idea.
Radiologists understand the potential value of a multimedia report for their referring colleagues. However, even if they had the available technology, they simply do not have time for an extra step, unless it is quick and easy. Some vendors offer the ability to add images to reports, but that can be cumbersome. Without tight integration, having separate applications from two different vendors can complicate the process of importing images from the viewer (i.e. PACS) into the reporting system.
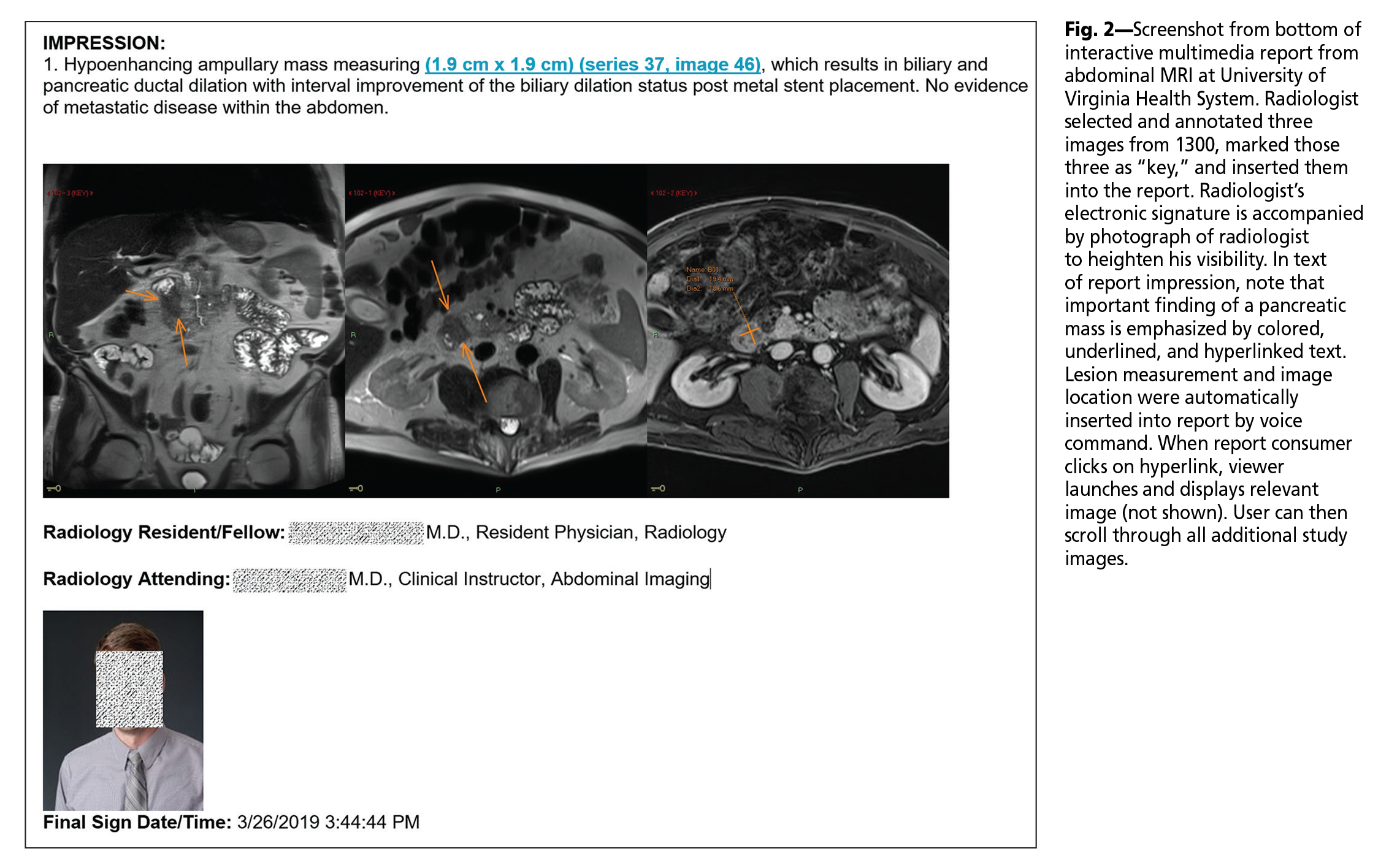
One solution is the hybridization of reporting and viewing applications into one. Because the systems are combined, the reporting system is more naturally aware of what is in the viewer, thus facilitating the import of key images. At the University of Virginia Health System (UVaHS), this approach (Vue PACS with Vue Reporting, Carestream Health) allows us to add images into our clinical reports [1]. The process is as follows: important images are optimized in the viewer, marked as “key” by a mouse click, and then a voice command inserts the images into the report (Fig. 2). The process only takes seconds to complete.
The concept of the reporting system being “aware” of what is in the viewer can be applied in additional ways. Radiologists routinely compare the study they are interpreting to relevant prior studies and dictate identifying details into their report. With the reporting system alert to prior studies opened in the PACS, a voice command can automatically insert details of these studies into the report. This can save time and reduce transcription error.
An even more important advancement is the ability to place hyperlinks within the report. This dynamic addition powers a variety of interactive elements through a URL to enhance the experience of those viewing the report, whether to a referring provider, downstream radiologist, or patient.
Consider the example where a radiologist annotates an image in the PACS, either by drawing an arrow pointing to a subtle finding or measuring a small lesion. A voice command inserts hyperlinked text into the report, carrying context from the last annotation made in the viewer. From the radiologist’s perspective, measurements, identifying series, and image numbers are automatically inserted into the report without dictating these details, again saving time and reducing transcription error. From the referring provider’s perspective, important findings stand out in the report as colored hyperlinked text that can provide immediate access to relevant images (Fig. 2). This could accelerate report and image review time, as well as improve report clarity.
At UVaHS, we have found this multimedia reporting approach to be enough of a departure from traditional plain-text-only reporting that it requires more than just access to the technology; it necessitates brief training and months or more for cultural adoption. Nevertheless, our radiologists now commonly create interactive multimedia reports for complex imaging studies like CT, PET/CT, and MRI. This elective change in care delivery indicates that our radiologists find value in the result.
Hyperlinks can further enhance reports by connecting to a variety of additional content beyond key imaging findings. Conceptually, once hyperlinks are supported, any content available via URL activation could be leveraged. For example, links within the report could be enabled to launch: secure sites to facilitate patient- and study-context email communication; a report grading system for providers or patients to contribute feedback; a webpage to share radiologist’s credentials; or a webpage with patient-friendly content to help the patient learn useful information about the examination.
Beyond the technological advancement needed to create interactive multimedia reports and the hurdle of cultural adoption by radiologists, another barrier to report evolution is the ability to distribute and view the advanced reports. It is routine for an electronic health record (EHR) to receive, archive, and display plain-text-only reports; however, the system may not be designed to handle more contemporary document formats, like RTF and PDF, to convey enriched content.
For the last couple of years at UVaHS, we have worked around this problemSH to enable our referring providers to access our advanced reports through the EHR in two ways. One is through a link to a PDF copy of the report stored in a document management system (OnBase, Hyland). The other is through a link to a lite digital viewer (Vue Motion, Carestream Health) that displays both the interactive multimedia report and all scrolling images from the study.
Recently, our EHR vendor (Epic Systems Corporation) completed development that should support interactive multimedia report content over an interface message in RTF format. We are collaborating with our vendors to test enriched report content directly within the EHR to increase viewing ease for clinicians.
We would also like for our patients to be able to see these advanced reports. If patients had an interactive report that allowed viewers to click on various findings and direct them to display the relevant images, patients may become more engaged with their imaging results and could develop a better understanding of their conditions. We are getting closer to this reality. As with many health care systems, our patients already can access their imaging results via a patient portal to the EHR. As a next step, we are working with our vendors to connect this patient portal to a patient-facing lite viewer that displays both radiology images and the interactive multimedia report.
In many aspects of daily life, digital communications are routinely enhanced beyond plain text with images, text formatting, and interactive elements. It seems natural to extend these improvements in communication to radiology reporting. We have already achieved technical success in doing so, and we have observed solid, sustained adoption by our radiologists. This is just the beginning. There are still challenges in distributing advanced reports, and referring providers are not even expecting to see them. This will change. In the future, interactive multimedia radiology reporting will likely become standard. Referring clinicians, and some discriminating patients, will come to expect enhanced reports. Radiologists will get used to creating them. Eventually, we will drop the words “interactive multimedia” and simply call them “radiology reporting.”
The opinions expressed in InPractice magazine are those of the author(s); they do not necessarily reflect the viewpoint or position of the editors, reviewers, or publisher.